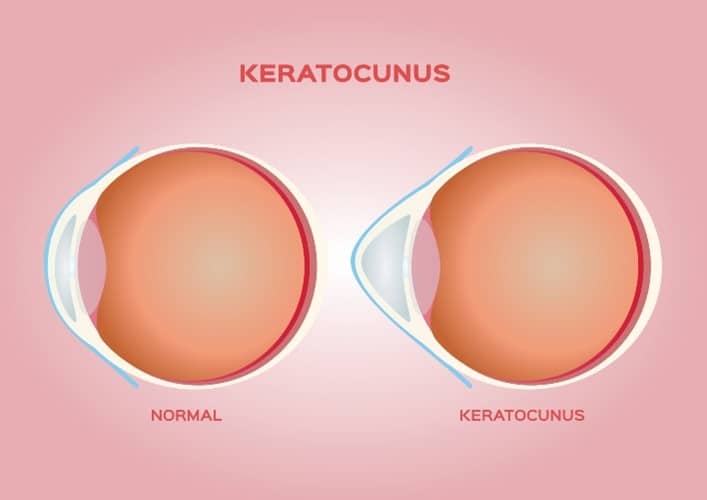
Keratoconus is an eye condition that causes the cornea — the transparent front surface of the eye — to get thinner and gradually bulge into a cone-like shape. This distortion inevitably impacts the vision, often leading to astigmatism or progressive myopia, which is a form of degenerative nearsightedness. Generally, keratoconus affects both eyes, though it can be more severe in one eye or not present in one eye altogether.
Keratoconus Symptoms
Most patients with keratoconus will first notice it in their teens and early 20s, and then see the condition get worse for the following decade. The earliest signs they tend to recognize are:
- Blurry vision
- Altered vision
- Light sensitivity
- Itchy eyes
If you discover that you have any of these symptoms, you should speak to an eye doctor as soon as possible. Early intervention is the best way to minimize the damage keratoconus can afflict on your sight.
Potential Causes of Keratoconus
Although ophthalmologists do not have conclusive proof of what causes keratoconus, research has linked the condition to a number of likely causes, which include:
- Eye allergies/itchy eyes
- Eye rubbing
- Genetics
- UV ray exposure from the sun
- Poor contact lens habits
- Imbalance of enzymes in the cornea
Corneal Crosslinking as Treatment
While keratoconus cannot be cured or reversed, patients can seek treatment to help prevent their eyesight from getting worse. The most recommended approach is corneal cross-linking. “Cross-linking” refers to the bonding that occurs among your eyes’ collagen fibers. These fibers link together to stabilize the cornea and slow it from bulging further.
Corneal cross-linking involves putting medicated riboflavin eyedrops on your cornea and then shining a custom UV light into the eyes for approximately half an hour to strengthen the corneal tissue. Because your eyes will be numbed with eyedrops, you should not experience any pain during this procedure.
Your doctor will apply topical anesthesia to numb the eye prior to the removal of the epithelium. This process helps prepare your eye so that the drug can penetrate the tissue of the cornea to have an effective iLink™ procedure. Today, this is the only cross-linking procedure deemed safe and effective by the United States FDA.
Risks
As with any medical procedure, there are some risks involved with corneal cross-linking:
- Eye discomfort
- Corneal damage
- Eye infection
- Blurry vision
Prior to your procedure, your ophthalmologist will confirm you are not an increased risk for these adverse side effects. Because the odds are low for most people, the benefits of protecting your eyesight generally outweigh these potential risks.
Caring for Your Eyes After Corneal Cross-Linking

Expect blurry vision and other disruptions to your vision in the initial days. As your eyes continue to heal in the coming months, many patients find that their eyes are sensitive to light; sunglasses can help with that.
Patients are instructed to wear special contact lenses to protect their eyes as they heal. In the event that this contact lens comes out, return to your doctor for attention. Do not attempt to replace it on your own.
The temptation to rub your eyes may be strong in the first week due to discomfort, but it is imperative not to rub them at all during this period. Instead, manage the discomfort with over-the-counter painkillers, or return to your doctor in the event that the pain is significant.
Does Insurance Cover Cross-Linking?
The medical necessity of FDA-approved iLink corneal cross-linking has become widely recognized, and as a result, the procedure is covered by over 96% of commercial insurance providers. Please contact your insurance carrier or your healthcare provider to understand any out-of-pocket costs you may be responsible for.
Seek Treatment for Keratoconus
If you suspect you have keratoconus or want to prevent your keratoconus from getting worse, the expert team at Boston Eye Physicians & Surgeons is here to help. Call (617) 232-9600 to book an appointment today.